Innovations for Development works with change agents in communities to provide analysis, facilitate collaborative learning, shape markets and support increased public-private engagement to strengthen health systems and reduce preventable maternal and child deaths.
The Challenge

Every year, more than six million children under age 5 die from preventable causes and nearly 300,000 mothers die from pregnancy- or childbirth-related causes (WHO 2016). High-impact interventions to reduce preventable maternal and child deaths exist, but they cannot be sustained within weak health systems.
Effective and resilient health systems are needed to ensure access to high-quality services for mothers and children across the continuum of care. Holistic health systems strengthening efforts combined with clinical- and community-based interventions can help to sustain reductions of and further decrease preventable maternal and child deaths.
Our Work
I4DEV’s approach to provide direct service delivery, strengthen health systems for maternal and child health services often begins with a focus on an individual system component like financing or health workforce. It also incorporates a holistic approach to ensure supportive management, governance and policy functions, which together produce sustainable improvements to the health system and, ultimately, to maternal and child health service delivery.
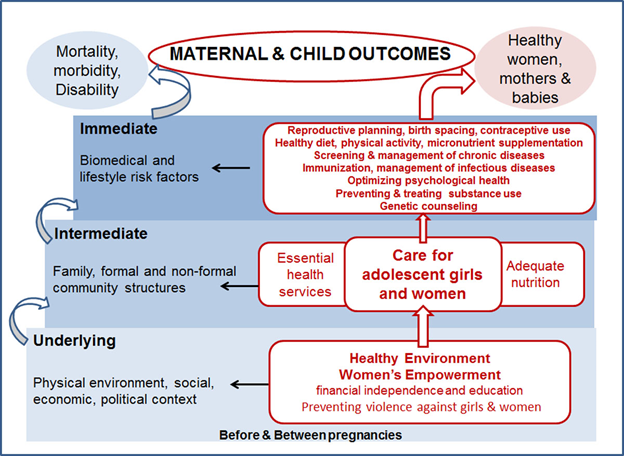
Our model to reduce maternal newborn and child mortality consists of improving coverage of effective integrated services at the different continuum of care. Starting with family planning, antenatal care (i.e. prenatal care) and treatment of anaemia, safe abortion, and postpartum care, the model includes both intrapartum interventions that reduce the incidence of a complication (e.g. misoprostol for postpartum haemorrhage [PPH], clean delivery for sepsis), as well as those that reduce the case fatality rate through appropriate management in a referral facility.
The interventions are geared at either reduce the incidence of complications or to reduce case-fatality rates associated with complications depends, in part, on access to specific services (e.g., trained Skilled Birth Attendants [SBA]) and to specific levels of facilities (e.g. comprehensive EmOC cEmOC] with capacity for blood transfusion).

Accordingly, the ultimate impact of our interventions depends on several setting-specific factors. These include delivery site, presence of birth attendant, quality and type of referral facility, as well as a successful referral when necessary. Our model therefore explicitly considers the location of delivery, type of assistance, access to basic or comprehensive obstetrical care, and the ability to overcome a series of barriers around the timing of delivery (e.g. recognition of referral need, reliable transport, timely treatment at an appropriate referral facility); these factors collectively determine the health services a woman can access and the specific interventions that would be included.
This model also allows us to evaluate phased approaches that involve scaling up access to services over time; the step-wise investments in infrastructure required to assure high-quality intrapartum care are designated as “upgrades.” In addition to reducing unmet need for family planning and unsafe abortion, four consecutively implemented strategies increased skilled attendants, improved antenatal/postpartum care, incrementally shift births away from home, and improve the availability and quality of EmOC for women delivering at home or in birthing centres. These also include improvement in the provision of referral need, access to transport, and expedient referral to an appropriate facility.
